Corneal Collagen Cross Linking
Corneal collagen cross linking was developed by Theo Seiler in 1998. This procedure can strength the front surface of the eye which is called cornea through the application of a special form of Vitamin B2 called Riboflavin to the cornea and this application is followed by exposing the cornea to Ultraviolet A light.
Riboflavin is a Photosensitizer that increase the chemical bonds and cross links between the collagen fibers in the cornea which helps to strengthen the cornea.
Steps of Corneal Collagen Cross Linking:
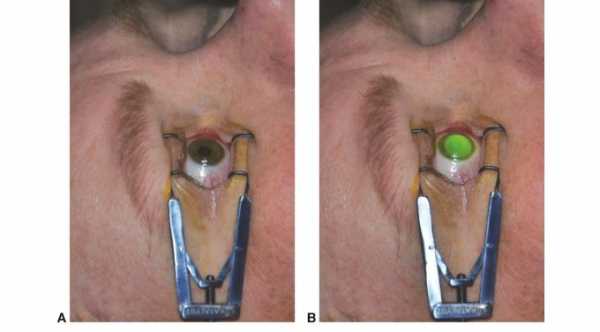
1- Removal of the superficial layer of the cornea that is called the epithelial layer. Removal of this layer helps the riboflavin to penetrate and diffuse deep into the corneal stromal layer.
2- A drop of yellow vitamin B2 (riboflavin 0.1%) is given for 20-30 minutes at an interval of 1-5 minutes.
3- Cornea is exposed for 20-30 minutes to Ultraviolet A light (365-370um) at a distance of 5 cm from the cornea.
Indications of Cross Linking
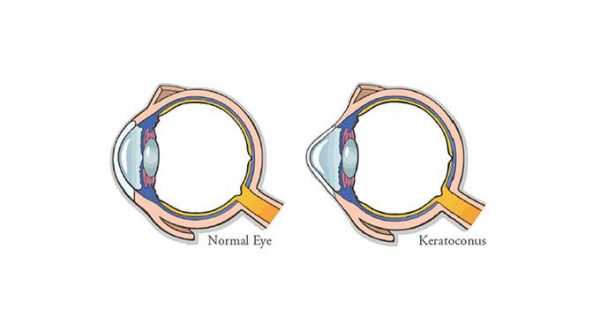
1- The main indication is corneal ectasia in which the cornea is weak and there is significant forward bulging of the cornea. This progressive bulging of the cornea increases corneal astigmatism and decreases the visual acuity.
Examples of corneal ectasia are keratoconus, pellucid marginal degeneration and ectasia after Lasik eye surgery. After cross linking, there is stabilization of corneal shape with no more forward bulging of the cornea and sometimes there is improvement in the visual acuity. Cross-Linking is the first option in keratoconus treatment.
2- Another indication which is still under research and study is corneal infection. Studies showed that patients with infective keratitis that is resistant to antibiotics eye drops can be treated with Corneal Collagen Cross Linking.
3- For the treatment of bullous keratopathy and corneal edema.
Best Candidates for Corneal Collagen Cross linking?
1- Age between 14 years and 35 years old. At the age of 14 years, there is a high risk of keratoconus progression. After the age of 35, there is natural cross linking between corneal collagen fibers. Studies showed that post cross linking complications are less in patients younger than 35 years.
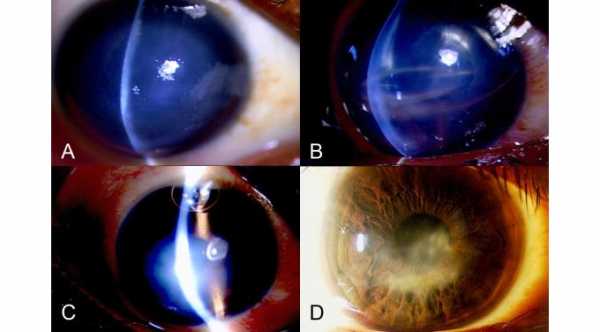
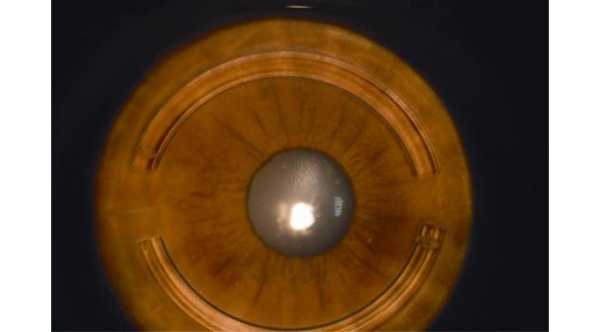
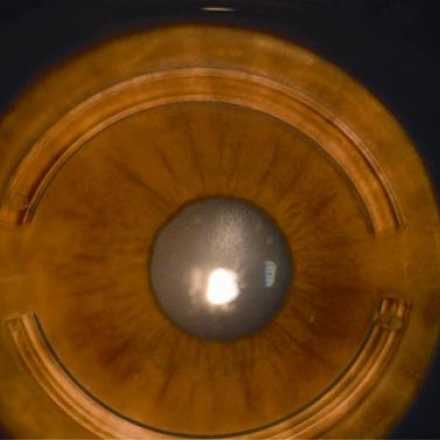
2- Clear Cornea at Slit Lamp examination with no scars or Vogt striae. Vogt Striae are wrinkles appear in the deep corneal stromal layer and they represent breaks in the descemet membrane and posterior stromal layer. The more Vogt Striae, the more severe is keratoconus.
3- Visual acuity is less than 20/25 because studies showed that complications after cross linking are more in patients with visual acuity of 20/25 or better.
4- Thickness of the cornea shouldn't be less than 400 μm.
5- Recently, A study showed that Cross Linking can stabilize Keratoconus in Children younger than 14 years and with no harm or side effects.
Transepithelial Cross Linking
Riboflavin can't pass through the epithelial layer of the cornea and in cross linking procedure, the corneal epithelial layer should be removed to allow the riboflavin to pass to the corneal stromal layers. New Modifications are applied to the molecular structure of the riboflavin to allow it to pass through epithelial layer of the cornea.
One modified Riboflavin is available in Europe and is called Ricrolin TE ( Ricrolin Transepithelium). This modification can help to reduce pain that is associated with epithelial removal and can prevent haziness that can occur with epithelial healing.
Corneal Cross Linking Shown to Improve Visual Acuity and Reduce Higher-Order Aberrations at the 2 Year Mark
Studies Show that Corneal collagen Cross Linking Really Does Work
In a study reported in Ocular surgery news 2014, corneal cross linking was shown to improve the overall vision and corneal shaping of 42 eyes tested. The interval of time between diagnosis of keratoconus and the cross linking treatment was, on average, 2.2 years.
The participants underwent topographical testing prior to the procedure and at 6 month intervals, up to 24 months following the procedure.
The findings of the topographical results were that the keratometry decreased, as well as the coma, trefoil, secondary astigmatism, secondary coma and secondary trefoil. In other words, the corneas of the test subjects were greatly improved by the cross linking procedure.
The resulting improved visual acuity, uncorrected, was due mainly to the improvements in the patients atypical keratometry, which is simple measurements of the steep and flat axis of the irregular astigmatism experienced by patients with keratoconus.
The improvement in corneal aberrations, due to the collagen cross linking procedure is now thought of as more of a refractive procedure than a treatment of any specific disease, which is debatable. Unlike patients who undergo Lasik as a cosmetic procedure to rid themselves of glasses, patients with keratoconus don’t have the luxury of picking up a pair of glasses and having near perfect vision.
In any event, the important point here is that there are options for patients suffering from keratoconus that have proven efficacy, according to the results of these studies.