Myopic Macular Degeneration
Myopic Macular Degeneration is a condition with excessive myopia with progressive expansion of the eye that is associated with formation of posterior staphyloma and severely blinding complications of the macula.
There are three categories of myopia; physiological, high and pathological myopia (myopic degeneration).
Physiological myopia has refractive error less than 6 diopters with axial length of less than 26 mm while high myopia has more than 6 diopters with axial length more than 26 mm.
Degenerative (Pathological) myopia is the same as high myopia with failure of stabilization of the axial length of the eye with progressive expansion and elongation of the globe. This expansion makes the sclera, choroid and retina thinner than those in normal eyes.
The causes of pathological myopia are unclear but both genetics and environmental factors can play a role.
Hereditary diseases such as Marfan syndrome, Stickler syndrome, Down syndrome and Ehlers-Danlos Syndrome can be associated with progressive myopia.
Ocular Features of Myopic Degeneration
1- Cornea
Corneal thinning and astigmatism.
2- Anterior Chamber and intraocular pressure
Anterior chamber is deeper than normal and there is high incidence of open angle glaucoma in these patients. Incidence of other types of glaucoma can be higher such as Pigmentary Dispersion Glaucoma and Steroid induced glaucoma.
3- Lens
Early formation of cataract especially nuclear sclerosis and posterior subcapsular cataract.
Degenerative myopia that is associated with systemic diseases such as Marfan syndrome and Ehlers-Danlos syndrome can also associated with zonular weakness which can lead to higher incidence of lens dislocation.
4- Vitreous Body
Posterior vitreous detachment and Vitreous syneresis at early age.
5- Retina, choroid and Sclera
- Higher incidence of Rhegmatogenous retinal detachment which can occur spontaneously, after ocular trauma or after cataract surgery. There is high incidence of Peripheral Lattice degeneration and atrophic holes which are risk factors for retinal detachment.
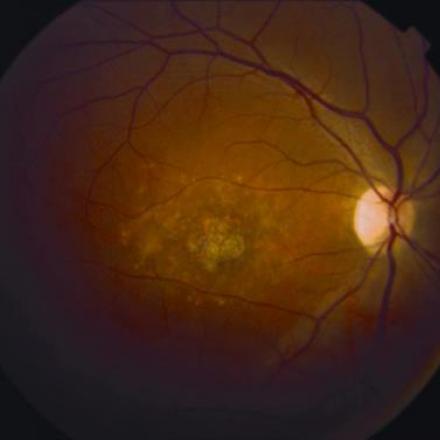
- Posterior Staphyloma. Localized Progressive expansion of the sclera accompanied by stretching and thinning of the choroid, retinal pigment epithelial and retina. Thinning of these layers gives a pale color of the fundus and the underlying blood vessels of the choroid can be visible. In severe myopic macular degeneration, even sclera can be seen.
- Progressive Choroidal and Retinal Pigment Epithelial atrophy. Atrophic area over the macular can severely affect central vision.
- Excessive stretching of Retinal pigment epithelium and Bruch’s membrane can cause the formation of microruptures which are called Lacquer Cracks. These microsuptures looks like yellow lines that are branching all over the posterior pole of the fundus. Lacquer Cracks can increase the incidence of Choroidal neovascular membrane formation.
- Choroidal Neovascular Membrane (CNV). It occurs mainly in areas with Lacquer Cracks. CNV that occurs in macular area can be associated with subretinal bleeding. Resolved hemorrhage can leave hyperpigmented scar which is called Fusch’s Spots.
- Macular Hole Formation
- Foveal Retinoschisis. Detachment within the retinal layer. It is different from Retinal detachment which is separation of the whole neurosensory retinal layer from the underlying retinal pigment epithelial and choroid while in Foveal Retinoschisis, the retina is attached to the underlying layer and the detachment occur within the retinal layers.
Treatment of Myopic Macular Degenerative
Myopic Macular Degenerative is one of the leading causes of legal blindness in the world. So far, the available treatment methods don’t offer cure and can’t stop the progression of it.
Regular follow up is required to detect any early changes or complications than can be treated such as glaucoma, cataract formation, retinal detachment and CNV.