Ocular Migraine
Ocular migraine, also known as ophthalmic or retinal migraine, is a condition causing temporary loss of vision or blindness. Unlike migraine with aura, ocular migraine affects only one eye. And in most cases, it happens in the same eye every time.
The exact cause of ocular migraine is unknown, but it has been linked to reduced blood supply to the eye due to narrowing or spasms of blood vessels. As the blood vessels relax, the blood flow becomes normal and vision is regained.
It is more common in women and people under 40 years old. A personal or family history of migraine increases one’s risk in having ocular migraine.
Ocular migraine symptoms
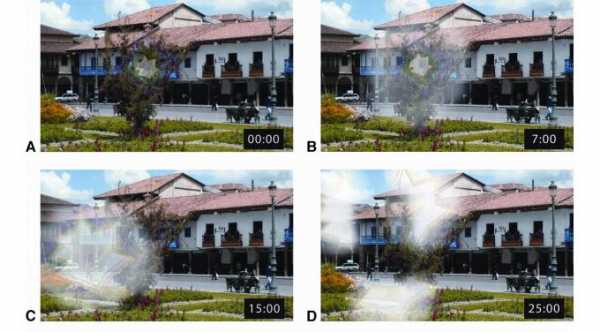
Partial or total loss of vision – affects one eye and lasts for 10 to 15 minutes up to an hour before gradually regaining vision. Some may see black patches or blind spots (scotoma) on their vision that may move or enlarge during the attack.
Headache– it may be present before, during, or after the visual disturbance and sometimes it can occur without headache (ocular migraine without headache)
Flashes of light and wavy, zigzag lines or halos around lights.
Other symptoms may include: Nausea, vomiting and/or sensitivity to sound and light
Diagnosis of Ocular Migraine
During an attack, the impaired blood flow to the eye may be seen under an ophthalmic instrument. But since it only lasts for a short time, diagnosis is likely to be based on your symptoms and history. Other diagnostic tests may be required to rule out other more serious conditions.
Ocular migraine prevention and treatments
An ocular migraine is typically harmless and it resolves on its own, so it usually doesn’t require any treatment. However, it is recommended to have an eye checkup if you experience any visual disturbance to rule out any other eye condition which might require immediate intervention.
Medication for treating migraines and to prevent future attacks may be prescribed by your doctor such as:
Pain reliever
Beta-blocker – may help to relax the blood vessels
Calcium channel blocker – may help prevent constriction of blood vessels
Aspirin – reduces pain and inflammation
Tricyclic anti-depressants and anti-seizure medications – may help prevent migraines
It may also help to take note of factors that might trigger migraine attacks, such as your activity or food prior to the attack, in order to prevent or reduce the occurrence of migraine.
Ocular Migraine Triggers
Stress
Certain foods
High blood pressure
Smoking
Low blood sugar
Exercise
Excessive heat
Dehydration
High altitude
Hormonal birth control pills
There is also a minor risk that the impaired blood flow may damage the blood vessels and the light-sensitive membrane inside the back of the eye (retina). It is rather rare but one thing that your doctor will monitor during your follow-ups.
What to do during an attack
Immediately STOP what you’re doing. If driving, pull over and do not continue driving until symptoms subside.
Relax and stay still. You may sit or lay down, whichever you are comfortable with.
Stay in a dark room and away from loud noises if possible.
Massage your head and temples to relieve pain.
Take medication for pain relief.
Seek medical advice.





