Ocular Examination for Lasik Eye Surgery
In order to know if you are a good candidate for lasik surgery or not, your doctor should perform complete eye examination and other diagnostic tests to determine if you are a good candidate for lasik or you are not.
Ocular Examination for Lasik Eye Surgery include:
1- Visual Acuity
Visual acuity, uncorrected and corrected and determine the best corrected vision. Standard and cycloplegic refraction of the eye to determine what type of refractive error you have. The range of refractive error that can be corrected be lasik is not more than ( 10 ) diopters for myopia, not more than ( 4 ) diopters of hyperopia and the range of astigmatism is (4-6) diopters.
2- Slit Lamp Examination
This step in ocular examination is very important. Slit lamp examination to determine the clarity of the cornea and if there is any corneal scar or damage and also to determine of there is cataract or anterior chamber disorders. Fundus examination should be done to rule out retinal diseases
3- Tonometry
Tonometry is an instrument that is used to measure intraocular pressure. There are many types of tonometry such as pneumatic tonometry, applanation tonometry and tonopen.
4- Pupil Size
Patient with very large pupil will have increase risk of glare and halos after lasik. Evaluation of pupil size should be done on both bright room and dark room. Ideally the area of the cornea that will be treated by laser should be larger than the pupil or you will have these symptoms.
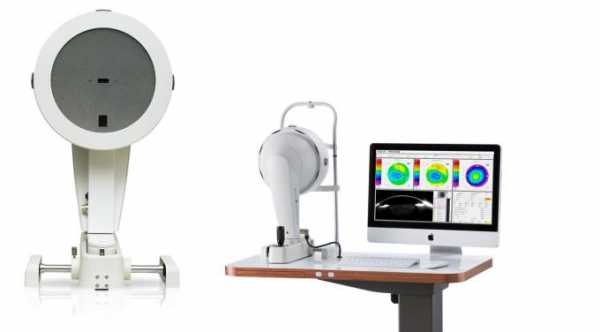
5- Corneal Topography or Corneal Mapping
Corneal topography is an important part in ocular examination before lasik surgery in which it will show the curvature of the cornea. The test helps to rule out keratoconus and any abnormal corneal curvature. The risk of irregular astigmatism and corneal flap complications are high in patients with keratoconus.
It is used also to confirm the stability of the cornea after discontinue the wearing of contact lenses. You should stop wearing soft contact lens at least 3-5 days before the corneal topography test and the hard contact lens should be stopped for at least 2 weeks before the test.
Corneal Topography can be very helpful to determine if the cornea is too steep or too flat as this can increase the risk of poor corneal flap creation.
6- Corneal Thickness or Corneal Pachymetry
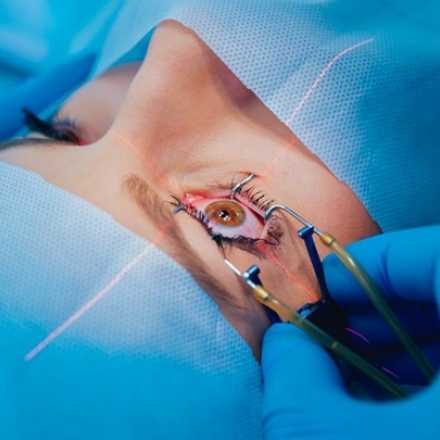
By this step in ocular examination, we will determine the thickness of the cornea and also we can determine how much the thickness of the flap and ablation depth should be.
The normal corneal thickness is around 500-550 microns and with lasik there will be creation of corneal flap with thickness of 120-180 microns. The remaining corneal bed should be at least 250 micron because with less than this thickness, the cornea will be thin and weak and with minor trauma it can be ruptured or get perforated easily and in long run with this weakness, the cornea will bulged outward in what is called corneal ectasia, which can cause changes in refractive power and high irregular astigmatism.
With thinner flap, the rate of flap complications like folds and wrinkles will be increased, but with intralase lasik in which your doctor will use laser femtosecond rather than mechanical microkeratome to create the flap, thinner flap can be created with fewer complications.
A study was conducted on mayo-clinic to see if there are outcomes differences in the final vision, side effects, or overall success rates of patients who had lasik with mechanical microkeratome and those patients who had lasik with laser femtosecond. The study came out with negligible difference between both surgeries but still there are many doctors prefer to do lasik with laser microkeratome because they believe that it is safer for flap creation.
When you have a thin cornea and your surgeon can not create a thin flap even with intralase lasik, you might not be a candidate for lasik but you can undergo PRK, Lasek or Epi-lasik. In these procedures there will be no flap creation and so minimize the risk of post-operative corneal ectasia with lasik.
7- Wavefront Analysis
We can use it to measure the refractive error and diagnosis of high order ablation and also for wavefront laser surgery which is custom lasik surgery or wavefront guided laser ablation of the cornea. Read more about wavefront analysis