Scleromalacia Perforans
The white of our eye is called as the ‘sclera’. It is the protective outer covering of eye containing the supporting tissues. Scleromalacia perforans is also known as Necrotising scleritis. The term scleritis means inflammation of the white of the eye.
The sclera of an eye is basically made to support the eye and it provides strength again from any damage. It is made up of the specialized tissue known as the collsgen connective tissue that gives protection to the underlying eyeball.
Types of Scleritis
Scleritis can be of two types:
1. Anterior scleritis
2. Posterior scleritis
Anterior scleritis affects the front parts of an eye, while the posterior scleritis involves the parts lying on the back of an eye.
Description
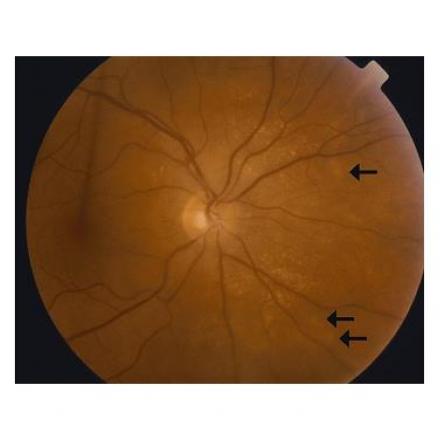
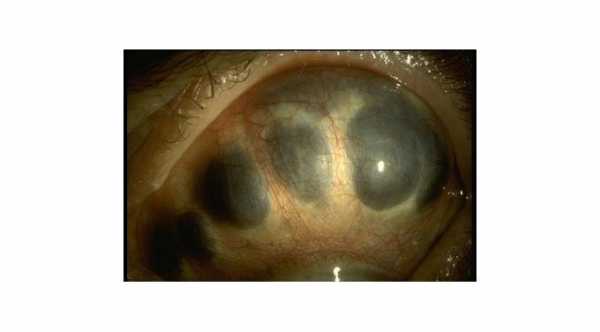
Scleromalacia Perforans is a condition comprising of severe thinning of the outer white layer of eye (sclera), but this type of scleritis occurs without any inflammation of the eye and is thus a painless condition until the complications occur. This thinning leads to protrusions of the underlying layer of the eye, called as the ‘Uvea’ or ‘Uveal tissue’.
The affected areas of the eye, having loss of the scleral tissue may show the underlying blood vessels crossing them. Most of the times this condition found associated with some other medical conditions like rheumatoid arthritis or other systemic illnesses. The good aspect regarding this disease is that it is very rare in occurrence. If left untreated, this disease can lead to blindness.
Signs and Symptoms of Scleromalacia Perforans
This disease is usually related to following symptoms:
1. Red eye.
2. Photosensitivity (increased sensitivity to light).
3. Excessive tearing or watering of eyes.
4. Blurred Vision.
5. Bluish hue in the affected eye.
It is a non-inflammatory condition of the eye and it does not cause any pain or inflammation.
Causes and Risk Factors of Scleromalacia Perforans
There may be several different causes for this disease, but about 50% of cases are usually reported to be associated with and underlying systemic illness like:
1. Rheumatoid arthritis.
2. Wegener’s granulomatosis.
3. Gout.
4. Systemic lupus erythematosis.
5. Polychondritis.
6. Ankylosing spondylitis.
7. Polyarteritis nodusa.
Age Group Affected
Most of the times the people affected with Scleromalacia Perforans lie within 30 – 60 years of age. It is very rarely found in children. Women are affected more commonly than men.
Diagnosis of Scleromalacia Perforans
If a person is suffering with any of such systemic illnesses like rheumatoid arthritis, systemic lupus erythematosus or other conditions listed above, and he develops the signs and symptoms involving his eyes, he must be checked by an ophthalmologist (doctor specialized for checking eyes).
The condition is diagnosed after specialized checkup via the slit lamp (special equipment using the light source and microscope which helps to examine the eye of the patient), torch or fundoscope which helps to confirm the diagnosis. Some blood tests may also be advised in an attempt to rule out the involvement of systemic illnesses.
Treatment of Scleromalacia Perforans
The usual treatment of Scleromalacia Perforans includes the use of both the topical and systemic medications. The topical treatment is in the form of eye drops and systemic treatment usually comprises of the steroids, non-steroidal anti-inflammatory drugs (NSAIDS) or the immunosuppressive drugs which suppress the body’s immune cells in order to halt the undergoing immune processes causing various illnesses.
Beside that, it is always mandatory to treat the associated diseases like rheumatoid arthritis or the others listed above with their specific medications, if the patient is suffering with any of them.
The course is followed in following manner:
1. The patient is initially given the immunosuppressive drugs along with the corticosteroids.
2. If the patient does not respond, then the immunosuppressive drugs are replaced by the other possible combinations.
3. It is always advised to avoid the subconjunctival and peri-ocular steroid injections as they may even lead to a further thinning of the sclera.
Surgical Treatment of Scleromalacia Perforans
The need for surgery rises in Scleromalacia Perforans when there is rupture or puncture of sclera due to extreme thinning. The surgical treatment is carried out by repairing the punctured areas with grafts taken from other parts of the patient’s body.
Complications of Scleromalacia Perforans
If this disease untreated or ignored, it can become complicated. As this is a condition resulting from thinning of the sclera, a severity of disease can lead to extreme thinning which can cause rupture or puncture of sclera. Such a condition requires an urgent surgical treatment.
Other complications include:
1. Blindness.
2. Inflammation of other parts of the eye including cornea (the transparent part of an eye), lens or uvea (the middle layer of an eye).
Prognosis and Outcomes
Scleromalacia Perforans has a good outcome provided the condition is diagnosed at an early stage and treatment started before any complication arises.